DOCTOR INFORMATION
Motivational Interviewing Techniques
Primary care practitioners face the challenge of helping patients to change their behaviour which poses significant risk, e.g. to their health. Motivational interviewing is a method of counselling which involves increasing the patient’s motivation to change. It is based on the principle that change is not a single event, it is a process. In this article we will explain: what it is; why it is necessary; some techniques; how to be successful; how to approach it; the four processes involved. At the end of each section you will find a useful summary of the most important information which you should remember.
An introduction to Motivational Interviewing
What is Motivational Interviewing❓
 Carl Rogers (1983) proposed a person centred approach to counselling and therapy 👵
Carl Rogers (1983) proposed a person centred approach to counselling and therapy 👵
 The motivational interviewing clinical method was developed from Rogers’ approach
The motivational interviewing clinical method was developed from Rogers’ approach
 Motivational interviewing strives to improve the patient’s motivation and in turn encourage them to commit to making a change 👍
Motivational interviewing strives to improve the patient’s motivation and in turn encourage them to commit to making a change 👍
 In this way, the patient is not being told what to do by a clinician, instead, they are telling themselves what they need to do ❗
In this way, the patient is not being told what to do by a clinician, instead, they are telling themselves what they need to do ❗
 Clinical trials have shown that motivational interviewing is associated with higher success rates than traditional treatment methods ✅
Clinical trials have shown that motivational interviewing is associated with higher success rates than traditional treatment methods ✅
 Adjusting your current consultation skills to incorporate motivational interviewing techniques can improve your own success rates ✅
Adjusting your current consultation skills to incorporate motivational interviewing techniques can improve your own success rates ✅
How does motivational interviewing work❓
 Motivational interviewing is a conversation style which strives to enhance a patient’s motivation to enact change
Motivational interviewing is a conversation style which strives to enhance a patient’s motivation to enact change
 You are exploring ambivalence and the patient’s readiness for change
You are exploring ambivalence and the patient’s readiness for change
 You should allow the patient to do most of the speaking 👩
You should allow the patient to do most of the speaking 👩
 Your role is to support them and help them understand their motivation to change 😊
Your role is to support them and help them understand their motivation to change 😊
 You should not act as the expert in the conversation, they know more about their situation than you do, and so, you should allow them to take the lead 👩
You should not act as the expert in the conversation, they know more about their situation than you do, and so, you should allow them to take the lead 👩
What types of situations can motivational interviewing be used in❓
 Any situation in which you change a patients mindset from one idea to another by helping them see the risks caused by their behaviour 👩
Any situation in which you change a patients mindset from one idea to another by helping them see the risks caused by their behaviour 👩
 E.g. addicitions (e.g. drugs, smoking and alochol abuse) 🍻
E.g. addicitions (e.g. drugs, smoking and alochol abuse) 🍻
 E.g. a patient who decides to undergo treatment for a disease or condition having previously being sceptical
E.g. a patient who decides to undergo treatment for a disease or condition having previously being sceptical
 E.g. weight loss/dieting/exercise 🚴
E.g. weight loss/dieting/exercise 🚴
 E.g. medication adherence 💊
E.g. medication adherence 💊
 E.g. School counsellors 🏫
E.g. School counsellors 🏫
 E.g. Management of pain 😖
E.g. Management of pain 😖
 E.g. Management of stress
E.g. Management of stress
 E.g. Completing recommended diagnostic tests/referral/screening 💉
E.g. Completing recommended diagnostic tests/referral/screening 💉
 E.g. Engaging is prevention programmes (diabetes/cardiovascular health)
E.g. Engaging is prevention programmes (diabetes/cardiovascular health)
Your role in motivational interviewing:
 Think about what the behaviour the patient exhibits means
Think about what the behaviour the patient exhibits means
 Explore how the patient is thinking about the benefits and challenges they may face when enacting change 😔
Explore how the patient is thinking about the benefits and challenges they may face when enacting change 😔
 Help the patient to prepare for the change 😊
Help the patient to prepare for the change 😊
 Provide encouragement to support the patient through the process of change, make them believe that the change is important and that they are capable of it 😊
Provide encouragement to support the patient through the process of change, make them believe that the change is important and that they are capable of it 😊
 Provide the patient with information at the correct point, when they are receptive to hearing more about the change 📃
Provide the patient with information at the correct point, when they are receptive to hearing more about the change 📃
 Set the patient small, realistic goals
Set the patient small, realistic goals
 Understand and accept that some patients will relapse
Understand and accept that some patients will relapse
Disadvantages of motivational interviewing:
 It is a time-consuming process, involving numerous consultations ⌛
It is a time-consuming process, involving numerous consultations ⌛
 Training is time-consuming and costs money 💵
Training is time-consuming and costs money 💵
Summary:
Motivational interviewing is a conversation-style which is used to enhance a patient's motivation for change. It can be used in the place of traditional consultation, in a range of situations, most commonly addiction e.g. alcohol/substance abuse. Your role is to support the patient through the process of change, by encouragement. However, it is time consuming, and so, costs money due to the number of consultations require.

Why is motivational interviewing necessary❓
What is the purpose of motivational interviewing❓
 Helps you to work collaboratively with the patient to decide what needs to be done 👭
Helps you to work collaboratively with the patient to decide what needs to be done 👭
 Stops you doing something, e.g. using inflammatory language, which will cause the patient to become defensive and close off 😠
Stops you doing something, e.g. using inflammatory language, which will cause the patient to become defensive and close off 😠
 Stops a difficult consultation becoming a challenge as you work together as a team
Stops a difficult consultation becoming a challenge as you work together as a team
Goals of motivational interviewing:
 Motivational interviewing aims to increase the effectiveness of behaviour change
Motivational interviewing aims to increase the effectiveness of behaviour change
 To combine motivational interviewing with the stages of change theory
To combine motivational interviewing with the stages of change theory
 You should make sure you understand the processes required for someone to change their behaviour ✅
You should make sure you understand the processes required for someone to change their behaviour ✅
 Motivational interviewing helps to minimise the frustration caused to the patient, and also to yourself 😠
Motivational interviewing helps to minimise the frustration caused to the patient, and also to yourself 😠
Patients are often ambivalent:
 There are usually many pros to changing a behaviour which poses risk, however, there are also often many cons perceived by the patient
There are usually many pros to changing a behaviour which poses risk, however, there are also often many cons perceived by the patient
 It is weighing up these pros and cons which most often causes patients to display ambivalence 😔
It is weighing up these pros and cons which most often causes patients to display ambivalence 😔
 Ambivalence is particularly significant in scenarios where the benefits of change are long term effects, whereas the short term consequences are perceived as cons
Ambivalence is particularly significant in scenarios where the benefits of change are long term effects, whereas the short term consequences are perceived as cons
Why do patients struggle with change❓
 Lack of motivation and confidence 😔
Lack of motivation and confidence 😔
 Being ‘told’ what to do actually make it more likely we will do the opposite
Being ‘told’ what to do actually make it more likely we will do the opposite
 Lack of determination/perseverance to change behaviour 😔
Lack of determination/perseverance to change behaviour 😔
 Procrastination (people often think about changes they will make a long time before doing so) ⌛
Procrastination (people often think about changes they will make a long time before doing so) ⌛
Summary:
Motivational interviewing is important as it builds rapport, helping you to work collaboratively with the patient to increase their will to change their behaviour. It reduces their ambivalence and procrastination. It has been proven that being told what to do is more likely to make us do the opposite.
Techniques for Motivational Interviewing
4 RULES for motivational interviewing:
 R: resist (the urge to instruct the patient how to change)
R: resist (the urge to instruct the patient how to change)
 U: understand (why this specific patient wants to change)
U: understand (why this specific patient wants to change)
 L: listen (to the patient with respect and interest) 👂
L: listen (to the patient with respect and interest) 👂
 E: empower (the patient to want to change and know that they have the ability to do so)
E: empower (the patient to want to change and know that they have the ability to do so)
5 principles of motivational interviewing:
 Display empathy 😊
Display empathy 😊
 Discuss and explore the discrepancy between the patient’s current situation and where they want to be
Discuss and explore the discrepancy between the patient’s current situation and where they want to be
 Do not engage in argument with the patient ❌
Do not engage in argument with the patient ❌
 Acknowledge resistance to explore it further, do not strengthen it ❌
Acknowledge resistance to explore it further, do not strengthen it ❌
 Support the patient’s view of their ability to enact the change ✅
Support the patient’s view of their ability to enact the change ✅
Processes involved in motivational interviewing:
- Engaging: listen to the patient empathetically 👂
- Focusing: make change the patient’s target
- Evoking: get the patient thinking, and discuss their ideas
- Planning: plan how change will be achieved 📃
What do you need to discuss in motivational interviewing❓
- Opening: discuss the patient’s lifetsyle habits, their substance use and stresses 💊
- Opening: discuss the patient’s health and use of substance 💊
- Ask about a typical day for the patient
- Discuss the pros and cons of the action which requires change ✅
- Give the patient information about the action when they are ready
- Discuss how the patient would like to be in the future and then discuss their present situation
- Discuss the patient’s concerns about their current behaviour
- Help the patient make a decision about what to do if they have decided to make a change to their behaviour 📃
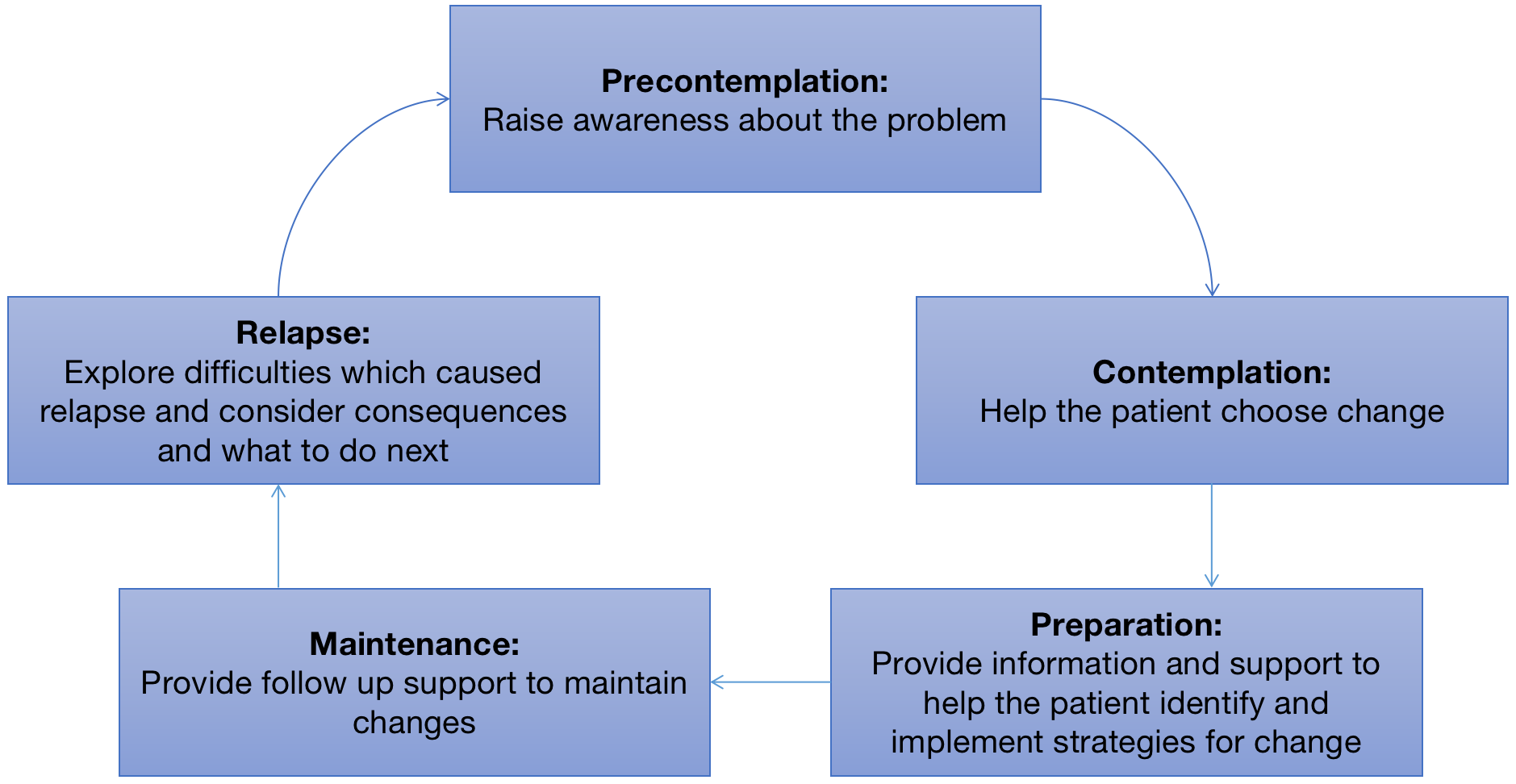
Stages of change model
 (Adapted from the work of Prochaska and DiCliemente)
(Adapted from the work of Prochaska and DiCliemente)
 This is a framework for understanding the processes involved in implementing change
This is a framework for understanding the processes involved in implementing change
 Progression through each stage of the model eventually leads to action and maintenance of this (the patient successfully making the desired change and maintaining this new behaviour) ✅
Progression through each stage of the model eventually leads to action and maintenance of this (the patient successfully making the desired change and maintaining this new behaviour) ✅
 Relapse, although not desirable should be viewed as a learning curve, to help the patient understand how to maintain the behaviour change
Relapse, although not desirable should be viewed as a learning curve, to help the patient understand how to maintain the behaviour change
Summary:
You should remember the 4 RULEs of motivational interviewing: resist, understand, listen, empower. You should follow the 5 principles: display empathy, explore discrepancies between current situation and goals, do not argue, acknowledge their resistance and and support them. You need to engage in the consultation, focus on their target, evoke their thoughts, and plan for change. Use the stages of change model to help a patient who is going through the process of change.
How to be successful in Motivational interviewing
Top tips for motivational listening:
 Develop discrepancy: between the patient’s behaviour at present, and their goals
Develop discrepancy: between the patient’s behaviour at present, and their goals
 Do not argue with the patient ❌
Do not argue with the patient ❌
 Be empathetic and listen carefully to what the patient says 👂
Be empathetic and listen carefully to what the patient says 👂
 Be optimistic and honest: try to show that you are being genuine so the patient feels respected and encourage them with optimism so they do not become defeated 😊
Be optimistic and honest: try to show that you are being genuine so the patient feels respected and encourage them with optimism so they do not become defeated 😊
 Identify the differences between the patient’s aims and current behaviour
Identify the differences between the patient’s aims and current behaviour
 Do not oppose any resistance, instead adjust your actions e.g. by discussing it ❌
Do not oppose any resistance, instead adjust your actions e.g. by discussing it ❌
 Discuss the change, what it is, why they want it etc. to reinforce it, encouraging them to choose to make the change
Discuss the change, what it is, why they want it etc. to reinforce it, encouraging them to choose to make the change
 Highlight where the patient is and where they want to be so they are motivated to change this❗
Highlight where the patient is and where they want to be so they are motivated to change this❗
 Be empathetic, non-judgemental, supportive, and non-argumentative 😊
Be empathetic, non-judgemental, supportive, and non-argumentative 😊
 Find success to acknowledge or good news to give the patient 😊
Find success to acknowledge or good news to give the patient 😊
 Provide the patient with any information necessary 📃
Provide the patient with any information necessary 📃
 Demonstrate that you understand what the patient is saying e.g. by summarising
Demonstrate that you understand what the patient is saying e.g. by summarising
 Avoid lecturing (if you feel you are begginning to lecture them, go back to asking questions about their thoughts and opinions) ❌
Avoid lecturing (if you feel you are begginning to lecture them, go back to asking questions about their thoughts and opinions) ❌
 Avoid cheerleading (you should go back to focusing on the change the patient is making) ❌
Avoid cheerleading (you should go back to focusing on the change the patient is making) ❌
 Help the patient through helplessness (you should agree that change is hard and help them remember their previous success) or resistance (you should not argue with them, but instead, summarise what they say)
Help the patient through helplessness (you should agree that change is hard and help them remember their previous success) or resistance (you should not argue with them, but instead, summarise what they say)
What do you need to do to be successful at motivational interviewing❓
 Let the patient decide change is necessary. Overcoming your desire to ‘fix’ them ❌
Let the patient decide change is necessary. Overcoming your desire to ‘fix’ them ❌
 Act as a guide for the patient, rather than the problem-solver 😊
Act as a guide for the patient, rather than the problem-solver 😊
 Remain neutral, regardless of your personal or professional opinion, you are consciously not using your position or knowledge to influence the patient’s actions
Remain neutral, regardless of your personal or professional opinion, you are consciously not using your position or knowledge to influence the patient’s actions
 Empower the patient so they are confident that they can make the changes 😊
Empower the patient so they are confident that they can make the changes 😊
Summary:
Make sure the patient chooses to change, not you. Act as a guide for them, rather than someone who will 'solve' their problems. Be neutral, and empower them to make the changes required or desired.

How to approach motivational interviewing
Asking open-ended questions:
 It is important to ask open ended questions to establish the feelings and thoughts of the patient ❗
It is important to ask open ended questions to establish the feelings and thoughts of the patient ❗
 They promote conversation on the patient’s side as they cannot answer with one word and must thus explain what they mean
They promote conversation on the patient’s side as they cannot answer with one word and must thus explain what they mean
 This means that the patient is doing most of the talking and in turn, reveal additional information without you having to directly ask for it
This means that the patient is doing most of the talking and in turn, reveal additional information without you having to directly ask for it
Useful questions to ask:
 How important, on a scale of 1 to 10, is making this change to you❓
How important, on a scale of 1 to 10, is making this change to you❓
 How confident, on a scale of 1 to 10, are you that you can successfully make this change❓
How confident, on a scale of 1 to 10, are you that you can successfully make this change❓
Use reflective listening:
 This is an important technique required for motivational interviewing ❗
This is an important technique required for motivational interviewing ❗
 It involves checking, instead of assuming that you know what the patient means
It involves checking, instead of assuming that you know what the patient means
 This builds rapport between clinician and patient 😊
This builds rapport between clinician and patient 😊
 It is very flexible so can be used in any scenario
It is very flexible so can be used in any scenario
 You should look out for verbal and non-verbal responses from the patient, to establish the possible meanings
You should look out for verbal and non-verbal responses from the patient, to establish the possible meanings
How to handle resistance:
 Resisitance in motivational interviewing is when the patient views the situation differently to you
Resisitance in motivational interviewing is when the patient views the situation differently to you
 This is a sign that you need to change the direction of conversation and listen to their viewpoint more closely 👂
This is a sign that you need to change the direction of conversation and listen to their viewpoint more closely 👂
 You should try to understand what the patient is thinking and make a decision from there 👂
You should try to understand what the patient is thinking and make a decision from there 👂
 Types of resistance: arguing, denying, interrupting and ignoring
Types of resistance: arguing, denying, interrupting and ignoring
 You should try to avoid provoking resistance, however, if you do, you can use it to your advantage by shifting their perspective and inviting them to propose the solution
You should try to avoid provoking resistance, however, if you do, you can use it to your advantage by shifting their perspective and inviting them to propose the solution
Non-empathetic responses to avoid:
 Directing/ordering: delivered with authority ❌
Directing/ordering: delivered with authority ❌
 Threatening/warning: suggesting there will be negative consequences if the patient does not follow your advice ❌
Threatening/warning: suggesting there will be negative consequences if the patient does not follow your advice ❌
 Premature/unsolicited advice: giving advice or suggestions based on your own experience or knowledge
Premature/unsolicited advice: giving advice or suggestions based on your own experience or knowledge
 Lecturing/arguing/using logic to persuade: this implies that the patient needs help to reason through the issue ❌
Lecturing/arguing/using logic to persuade: this implies that the patient needs help to reason through the issue ❌
 Preaching/telling the patient their duty: telling the patient what they should or should not do
Preaching/telling the patient their duty: telling the patient what they should or should not do
 Judging/blaming/criticising: implies that the actions of the patient are wrong
Judging/blaming/criticising: implies that the actions of the patient are wrong
 Praising/agreeing: you should not give unsolicited agreement as it can disrupt the communication process 😊
Praising/agreeing: you should not give unsolicited agreement as it can disrupt the communication process 😊
 Mocking/shaming: disapproval suggests you intend to correct a patient’s thoughts or behaviour ❌
Mocking/shaming: disapproval suggests you intend to correct a patient’s thoughts or behaviour ❌
 Analysing/interpreting: you should not analyse or make assumptions about what the patient has said or thinks
Analysing/interpreting: you should not analyse or make assumptions about what the patient has said or thinks
 Questioning/probing: it is useful to ask some questions, however too many can interrput the communication flow between you and the patient ❌
Questioning/probing: it is useful to ask some questions, however too many can interrput the communication flow between you and the patient ❌
 Changing the subject/using humour: it is important to discuss the matter at hand, humour can distract from this
Changing the subject/using humour: it is important to discuss the matter at hand, humour can distract from this
How to develop discrepancies:
 Ask the patient to imagine the worst case scenario if they do not change their behaviour
Ask the patient to imagine the worst case scenario if they do not change their behaviour
 Ask the patient to imagine the best case scenrio if they try to chnage their behaviour
Ask the patient to imagine the best case scenrio if they try to chnage their behaviour
 Ask the patient to imagine their future with changed behaviour
Ask the patient to imagine their future with changed behaviour
 Ask the patient to think about their past when their behaviour was different to present, and how they wish to get it back to
Ask the patient to think about their past when their behaviour was different to present, and how they wish to get it back to
 Ask the patient about their behaviours which do not support their goals to change, do not accuse or judge the patient though ❌
Ask the patient about their behaviours which do not support their goals to change, do not accuse or judge the patient though ❌
 Reflect on the contradictions in what the patient says, using a supportive tone e.g. “ On one hand you are telling me that you want to change, but on the other you have told be why this is difficulty. It could be the case that the freedom to behave as you do now is so important to you that you are still prepared to deal with the consequences caused.”
Reflect on the contradictions in what the patient says, using a supportive tone e.g. “ On one hand you are telling me that you want to change, but on the other you have told be why this is difficulty. It could be the case that the freedom to behave as you do now is so important to you that you are still prepared to deal with the consequences caused.”
How to react to resistance:
 You can turn resistance into a new momentum towards change
You can turn resistance into a new momentum towards change
 Do not oppose resistance ❌
Do not oppose resistance ❌
 Avoid arguments in favour of the patient changing their behaviour ❌
Avoid arguments in favour of the patient changing their behaviour ❌
 Use resistance as a sign that you need to change your approach
Use resistance as a sign that you need to change your approach
 E.g. “From what you are telling me, it sounds like you have tried to change your behaviour and it has not worked”
E.g. “From what you are telling me, it sounds like you have tried to change your behaviour and it has not worked”
How to display empathy:
 Try to understand the opinions and feelings that the patient currently holds, and show that you understand them
Try to understand the opinions and feelings that the patient currently holds, and show that you understand them
 “What you are saying is very important to me, could you tell me more about...”
“What you are saying is very important to me, could you tell me more about...”
How to support self efficacy:
 You should support the patient’s belief in their own ability to enact the change desired
You should support the patient’s belief in their own ability to enact the change desired
 This is a strong motivator which will increase the chance of success ⬆
This is a strong motivator which will increase the chance of success ⬆
 If the patient feels as though you believe they have the ability to make the change, the patient will believe in themself more
If the patient feels as though you believe they have the ability to make the change, the patient will believe in themself more
 “What do you think will be the first step towards this change”
“What do you think will be the first step towards this change”
‘Dance don’t wrestle’:
 This phrase is used a lot when discussing motivational interviewing
This phrase is used a lot when discussing motivational interviewing
 It means do not fight or argue with the patient, work together, like a dance partner to achieve the patient’s goals ❌
It means do not fight or argue with the patient, work together, like a dance partner to achieve the patient’s goals ❌
 Do not be aggressive or forceful 😠
Do not be aggressive or forceful 😠
Summary:
You need to ask open-ended questions to allow the patient to do most of the speaking and decide to change for themself. Use reflective listening; be empathetic; develop the discrepancies between their current behaviour and their plans. Support self-efficacy and remember to 'dance not wrestle' with the patient.
Four Processes of motivational Interviewing:
Engaging:
 You should build rapport with the patient 😊
You should build rapport with the patient 😊
 Focus on the process more than the outcome 😊
Focus on the process more than the outcome 😊
 Try to promote the patient buying into the process of change ⬆
Try to promote the patient buying into the process of change ⬆
 Use the OARS technique
Use the OARS technique
Building rapport:
 Meeting 1:
Meeting 1:
- Welcome the patient and make sure they feel comfortable 😊
- Ask what their concerns and priorities are
- Explain what your role is
- Review a plan for the next time you meet 📃
 Meeting 2:
Meeting 2:
- Make casual conversation with the patient so they are relaxed 😊
- Explain what your goals are this time
- Ask them what they would like to discuss
- Follow up on what has happened since last time
- Review a plan for the next time you meet 📃
OARS skills:
 O: open-ended question (guide the conversation with questions which require more than a one word answer)
O: open-ended question (guide the conversation with questions which require more than a one word answer)
 A: affirmations (build their confidence by saying anything positive you notice about the patient e.g. successes) 😊
A: affirmations (build their confidence by saying anything positive you notice about the patient e.g. successes) 😊
 R: reflections (reflect on what the patient is thinking and feeling then repeat it back to them) - this is the most important skill for motivational interviewing 😊
R: reflections (reflect on what the patient is thinking and feeling then repeat it back to them) - this is the most important skill for motivational interviewing 😊
 S: summary (summarise what the patient says to show you have been listening and guide them towards the behaviour change needed)
S: summary (summarise what the patient says to show you have been listening and guide them towards the behaviour change needed)
Focusing:
 Keep the conversation focused on the change 😊
Keep the conversation focused on the change 😊
 Clarify what the patient sees as their priorities and how well prepared they are for the change
Clarify what the patient sees as their priorities and how well prepared they are for the change
 Use collaborative language in your conversation e.g.”we” 👭
Use collaborative language in your conversation e.g.”we” 👭
 Do not focus on areas which the patient is ambivalent about
Do not focus on areas which the patient is ambivalent about
 Action plans can be very useful for staying focused
Action plans can be very useful for staying focused
 Use agenda mapping to stay on topic 📃
Use agenda mapping to stay on topic 📃
 Consider the dilemma that the patient faces (their goals vs the potential consequences)
Consider the dilemma that the patient faces (their goals vs the potential consequences)
Evoking:
 Explore the patient’s motivations for wanting to change their behaviour
Explore the patient’s motivations for wanting to change their behaviour
 Use change talk (client speech which promotes change) 😊
Use change talk (client speech which promotes change) 😊
 Use OARS skills to explore their motivations and priorities 📃
Use OARS skills to explore their motivations and priorities 📃
 Ask questions to establish any potential barriers to the success of the patient changing their behaviour, and their past successes
Ask questions to establish any potential barriers to the success of the patient changing their behaviour, and their past successes
 Prepare for the change process: set goals by specific dates, give the patient relevant information or resources etc. 📃
Prepare for the change process: set goals by specific dates, give the patient relevant information or resources etc. 📃
 Explore the advantages and disadvantages of changing their behaviour by asking questions about their thoughts
Explore the advantages and disadvantages of changing their behaviour by asking questions about their thoughts
Change Talk (EARS):
- E) Explore: “What do you think would be the benefits of changing your behaviour?”
- A) Affirm: “It is a very big and positive step that you have decided to change your behaviour”
- R) Reflect: “So making this change could significantly affect...” 😊
- S) Sumarise: “You have given a lot of reasons to change yur behaviour such as...”
Planning:
 Develop a plan for how this patient is going to achieve their goals of changing their behaviour 📃
Develop a plan for how this patient is going to achieve their goals of changing their behaviour 📃
 Identify change talk, questions about changing, and less talk about barriers, as this is a sign that the patient is motivated to change their behaviour
Identify change talk, questions about changing, and less talk about barriers, as this is a sign that the patient is motivated to change their behaviour
 Make the plan collaboratively with the patient 👭
Make the plan collaboratively with the patient 👭
 Produce a structured plan which allows the patient to take responsibility for changing their behaviour and rewards them for meeting goals 📃
Produce a structured plan which allows the patient to take responsibility for changing their behaviour and rewards them for meeting goals 📃
SMART Planning:
- S) Specific: make sure goals are specific and not open to interpretation 📃
- M) Measurable: set goals which can easily be measured, e.g. a certain amount of weight loss
- A) Achievable: make sure the patient will be able to achieve the goals, as otherwise their morale will be lowered
- R) Realistic: goals must be realistic and not completely unattainable or something which will cause the patient to exert too much effort that they lose interest 📃
- T) Timely: ensure that the time between each goal is appropriate, you do not want to rush the process nor drag it out too long which will cause the patient to become tired of it
Summary:
The 4 most important processes of Motivational Interviewing are: engagement (build rapport with the patient), focusing (do not let the conversation go off topic), evoking (get the patient thinking about their motivations for change) and planning (make a plan for how the patient will make the change).
Summary:
- Motivational interviewing is a conversation-style used to enhance a patient's motivation for change
- It is a collaborative method in which you should work with the patient to increase their will to change their behaviour
- There are numerous models such as the stages of change models which should be used to guide motivational interviewing
- You need to do 4 things: 'engage' the patient by discussing their motivations, 'focus' the conversation on their behaviour and how to change it, 'evoke' feelings and thoughts by encouraging change-talk, 'plan' how the patient will change their behaviour
- Remember to be empathetic and non-judgemental!













