DOCTOR INFORMATION
Hypertension (for doctors)
How do you diagnose Hypertension❓
 Measure blood pressure (BP) using a suitably sized cuff
Measure blood pressure (BP) using a suitably sized cuff
 Measure the BP in both arms for comparison (if difference >15mmHg, repeat and if difference is still >15mmHg, use arm with higher BP going forward)
Measure the BP in both arms for comparison (if difference >15mmHg, repeat and if difference is still >15mmHg, use arm with higher BP going forward)
 If the BP is ≥140/90, repeat a 2nd time and a 3rd time if significant difference (lowest of final 2 readings is the relevant measurement)
If the BP is ≥140/90, repeat a 2nd time and a 3rd time if significant difference (lowest of final 2 readings is the relevant measurement)
| Clinic BP | Diagnosis | Action |
| <140/90 | Normal blood pressure |
|
| 140/90 to 179/119 | Hypertension |
|
| ≥180/120 | Severe Hypertension |
|
What is the criteria for patient referral❓
 Same day referral: accelerated hypertension/ phaeochromocytoma suspected
Same day referral: accelerated hypertension/ phaeochromocytoma suspected
 Routine referral: patients <40 with hypertension/ secondary hypertension suspected/ no response to step 4 of treatment ❌
Routine referral: patients <40 with hypertension/ secondary hypertension suspected/ no response to step 4 of treatment ❌
How is Postural Hypotension diagnosed❓
 Check BP when patient is seated, then repeat when standing
Check BP when patient is seated, then repeat when standing
 If systolic BP is >20mmHg lower, it indicates postural hypotension
If systolic BP is >20mmHg lower, it indicates postural hypotension
 Patients who are ≥80, have type 2 diabetes or symptoms such as dizziness should be tested for postural hypotension
Patients who are ≥80, have type 2 diabetes or symptoms such as dizziness should be tested for postural hypotension
 If postural hypotension is diagnosed, review patient’s drugs and use standing BP going forwards
If postural hypotension is diagnosed, review patient’s drugs and use standing BP going forwards
Management of Hypertension
First line drugs:
 First line drug is chosen depending of 3 factors: type 2 diabetes, ethnicity and age:
First line drug is chosen depending of 3 factors: type 2 diabetes, ethnicity and age:
 Type 2 diabetes: for ALL type 2 diabetes patients, use ACE inhibitor unless contraindicated
Type 2 diabetes: for ALL type 2 diabetes patients, use ACE inhibitor unless contraindicated
 African/African Caribbean ethnicity: for all patients excluding those with type 2 diabetes, use a calcium channel blocker unless contraindicated (if heart failure/oedema, use thiazide-like diuretic for BP control instead)
African/African Caribbean ethnicity: for all patients excluding those with type 2 diabetes, use a calcium channel blocker unless contraindicated (if heart failure/oedema, use thiazide-like diuretic for BP control instead)
 Patients <55 not of African/African Caribbean ethnicity: ACEi or ARB is ACEi is not tolerated
Patients <55 not of African/African Caribbean ethnicity: ACEi or ARB is ACEi is not tolerated
 Patients ≥55 who are not type 2 diabetics: thiazide-like diuretics
Patients ≥55 who are not type 2 diabetics: thiazide-like diuretics
Second line drugs:
 Any 2 of: ACE/ARB, CCB, thiazide-like diuretic 💊
Any 2 of: ACE/ARB, CCB, thiazide-like diuretic 💊
 Heart failure/oedema: ACE and thiazide-like diuretic should be used to control BP 💊
Heart failure/oedema: ACE and thiazide-like diuretic should be used to control BP 💊
 African/African Caribbean ethnicity: ARB instead of ACE
African/African Caribbean ethnicity: ARB instead of ACE
Third line drugs:
 ACE/ARB and CCB and thiazide-like diuretic
ACE/ARB and CCB and thiazide-like diuretic
Fourth line drugs:
 Resistant Hypertension: BP still not within target range, even after third line drugs ❌
Resistant Hypertension: BP still not within target range, even after third line drugs ❌
 Confirm elevation of BP with ABPM/HBPM
Confirm elevation of BP with ABPM/HBPM
 Assess for postural hypotension (as described above)
Assess for postural hypotension (as described above)
 Patient potassium ≤4.5: add spironolactone 25mg/d 💊
Patient potassium ≤4.5: add spironolactone 25mg/d 💊
 Patient potassium >4.5: consider addition of alpha/betblocker 💊
Patient potassium >4.5: consider addition of alpha/betblocker 💊
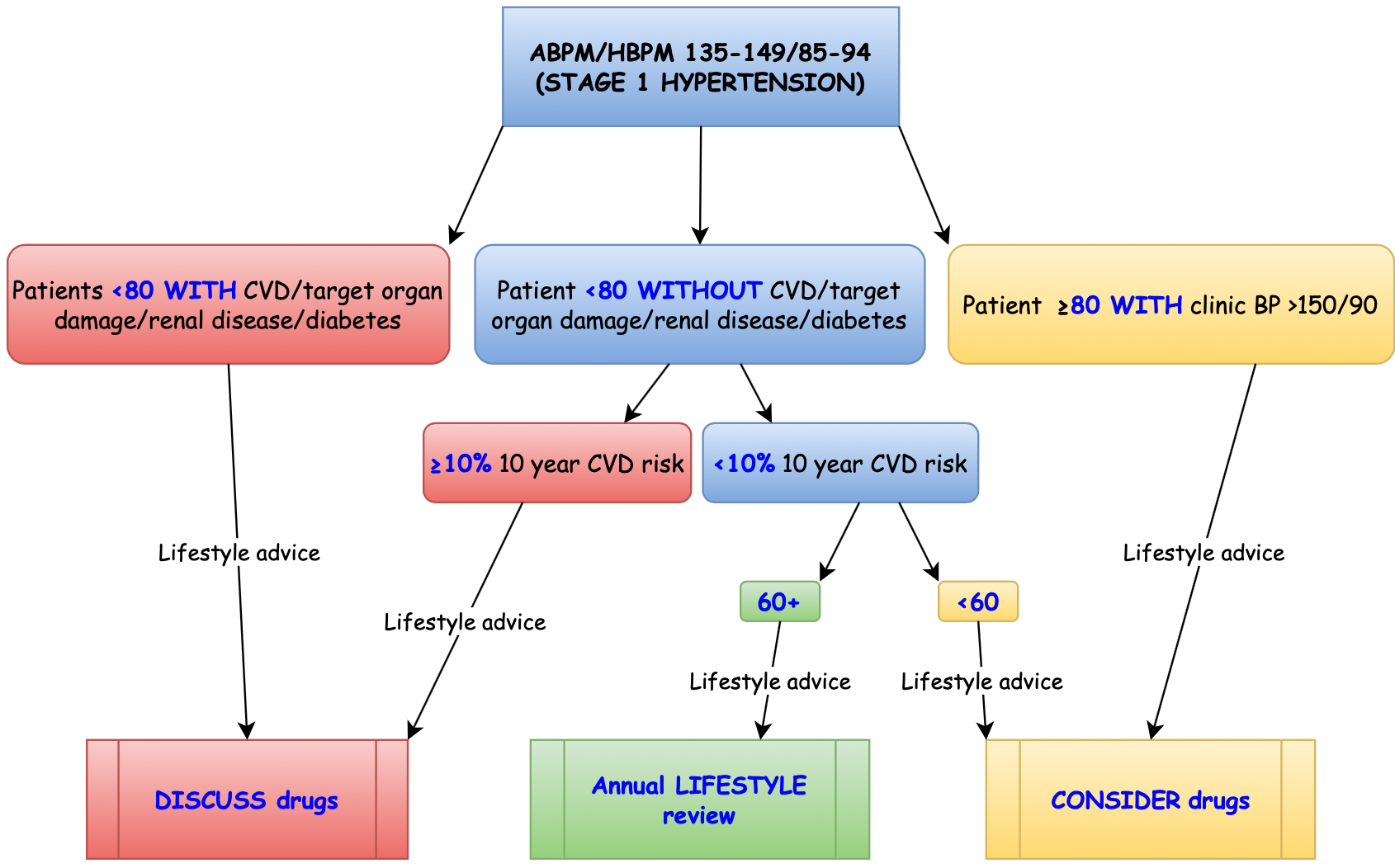
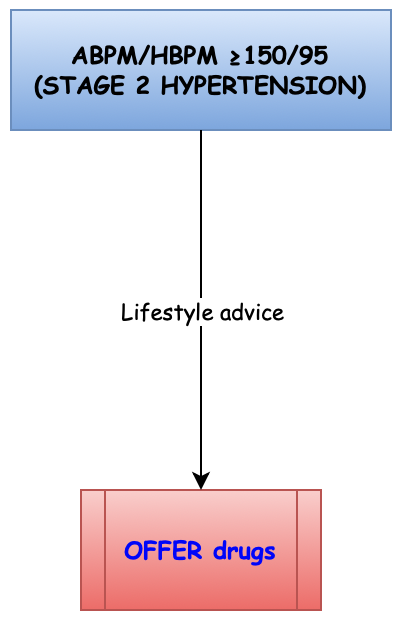
What are the targets of treatment❓
 Patients <80: clinic (140/90), ABPM/HBPM (<135/85)
Patients <80: clinic (140/90), ABPM/HBPM (<135/85)
 Patients ≥80: clinic (<150/90), ABPM/HBPM (<145/85)
Patients ≥80: clinic (<150/90), ABPM/HBPM (<145/85)
 If BP still not controlled after fourth line therapy: REFER the patient ❌
If BP still not controlled after fourth line therapy: REFER the patient ❌













